What is a Thyroid Lump or Nodule?
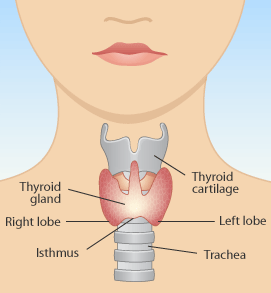
The thyroid gland is located on the lower front portion of the neck. It produces thyroid hormone, which simply put, regulates the production of energy in your body. A healthy thyroid gland is shaped like a butterfly, with the right and left lobes connected by a bridge called the isthmus.
Nodules or lumps occur commonly in the thyroid gland. It has been shown that 5% of the general population have a thyroid lump which can be found on clinical examination while up to 30-40% of the population have a thyroid nodule which cannot be felt but can be identified by ultrasound examination. Thyroid nodules occur much more commonly in women. The good news is that the vast majority of these nodules are benign or non-cancerous, with only approximately 10% of all thyroid nodules being found to be malignant or cancerous. Occasionally there may be multiple nodules in the thyroid gland in a condition known as multinodular goitre. When these nodules become very big, this can result in compression of the trachea (or windpipe), or oesophagus to cause breathing or swallowing difficulties. Cancers which occur in the thyroid gland are categorized as papillary and follicular carcinoma, medullary carcinoma, and rarely lymphoma or anaplastic carcinoma.
What are the worrying symptoms and signs for a thyroid nodule?
While the majority of thyroid nodules are non-cancerous and do not cause any discomfort to the patient apart from a lump in the centre of the neck, there are several symptoms and signs which are more worrisome for the possibility of a thyroid cancer. These include:
- Large size of the thyroid nodule (more than 4 cm)
- A nodule which is growing rapidly
- A nodule which is hard and painless
- Fixation of the nodule to the overlying skin or underlying deep neck structures
- Presence of a hoarse voice
- Difficulty in swallowing due to the nodule
- Presence of other enlarged lymph nodes in the neck
- If the patient is very young (less than 20 years old) or older (more than 60 years old)
- If the patient has a strong family history of thyroid cancer
- If the patient has previous exposure to radiation
What tests are necessary if I have a thyroid nodule?
Your doctor will usually take a full history and do a complete examination of the thyroid nodule and rest of the neck. A blood test known as the thyroid function test will be done to measure the levels of thyroid hormone in the blood to rule out hyper- or hypo-thyroidism. These conditions can occur if the thyroid gland or nodule is producing too much or too little thyroid hormone. A fine needle aspiration cytology (also known as an FNAC) test is routinely performed for a thyroid nodule. This biopsy test is done by using a very fine needle to remove cells from the lump. It is similar to an injection, causes very little pain and is routinely done in the clinic without the need for any local anaesthesia. The cells are then examined under a microscope to look for the presence of cancer cells. If there are no cancer cells seen, your doctor may choose to monitor the thyroid nodule and watch closely for any changes in size. Occasionally an ultrasound test is useful to assess for the presence of multiple nodules within the thyroid gland, or to monitor the size of the nodule.
What to expect in thyroid surgery?
The thyroid gland is located on the lower front portion of the neck (Fig 1). It produces thyroid hormone, which simply put, regulates the production of energy in your body. A healthy thyroid gland is shaped like a butterfly, with the right and left lobes connected by a bridge called the isthmus. Depending on the reason for surgery, all or part of the thyroid gland may be removed. Nodules or lumps are commonly found in the thyroid gland and the majority of these nodules are benign or non-cancerous. Occasionally there may be many nodules in the thyroid gland in a condition known as multinodular goitre. This can result in compression of the trachea (or airway), or oesophagus to cause breathing or swallowing difficulties. Cancers can also occur in the thyroid gland, including papillary and follicular carcinoma, medullary carcinoma, and rarely lymphoma or anaplastic carcinoma.
Why do I need thyroid surgery (also known as a thyroidectomy)?
You will usually be advised to have a thyroidectomy for one or more of the following reasons:
- Removal of a malignant (cancerous) or benign (non-cancerous) thyroid tumour.
- Treatment of thyrotoxicosis, in which an overactive thyroid gland is producing extremely high levels of thyroid hormone.
- Removal of part or all of a multinodular goitre which is pressing on neighbouring structures in the neck such as the trachea or oesophagus.
- To remove and evaluate an undiagnosed thyroid mass.
What happens during the procedure of thyroid surgery?
The thyroid operation involves delicate surgery and usually takes 1-2 hours depending on the size of the thyroid nodules or goitre. You will be administered general anaesthesia which means you will be unconscious for the whole operation. The operation is usually performed through an incision on the front of your lower neck in one of the natural skin lines. These incisions normally will heal very well without any problems or obvious scars.
You may have one or two wound drains to collect excess fluid which normally occurs after your thyroid surgery. The drains are small plastic tubes which are inserted at the end of the operation and are connected to a plastic collection bottle. The drains are not painful and you can carry them around with you. These tubes are usually removed 2-3 days after the operation and most patients are discharged home the day after surgery with these tubes. You will then return to the ENT centre for removal of these drains.
What to expect after thyroid surgery?
Most patients will be admitted to the ward for observation after surgery. Your length of stay in hospital will depend on the extent of your surgery. Many patients who have partial thyroidectomy will only require an overnight stay, whereas patients who had their entire thyroid glands removed may stay between 2-4 days.
You may experience temporary post-operative symptoms. These include:
- Drowsiness and nausea
- Neck pain and discomfort
- Pain on swallowing
You will be given painkillers for 5-10 days, and these symptoms usually will disappear after 1-2 days. The majority of patients will experience minimal symptoms after 1 day and are able to eat normally the evening after thyroid surgery.
What are some of the risks of thyroid surgery?
Thyroidectomy is generally a safe surgical procedure. However some patients may experience minor complications. These include:
- Hoarseness. The voice box and its nerves are closely related to the thyroid gland and may be affected during surgery. If this happens, you may notice a change in your voice. This is usually temporary should it happen, and most patients will have a full recovery of their voice after a few weeks. It is important that the surgeon identify the nerves confidently to prevent accidental damage.
- Hypocalcaemia. The parathyroid glands which control the blood calcium levels are also closely located next to the thyroid gland, and may be affected during surgery, especially when the entire thyroid is removed. If this happens, the blood calcium levels will fall and you may experience numbness, tingling or cramps of the face, hands and feet. This can be easily treated by giving calcium supplements, either by intravenous drip and/or by tablets. However this complication can be prevented by carefully dissecting the parathyroid glands during surgery.
Useful links:
http://www.thyroid.org/patients/faqs.html
http://www.british-thyroid-association.org/info-for-patients/
Please contact us if you have further enquiry on Thyroid Lumps and Disorders or Request an appointment to see our ENT specialist