At least a quarter of the general population have habitual snoring, while occasional snoring is almost universal. Snoring can be a pain – for your sleeping partner that is, who is kept awake by the noise.
Why people snore? Or What causes snoring?
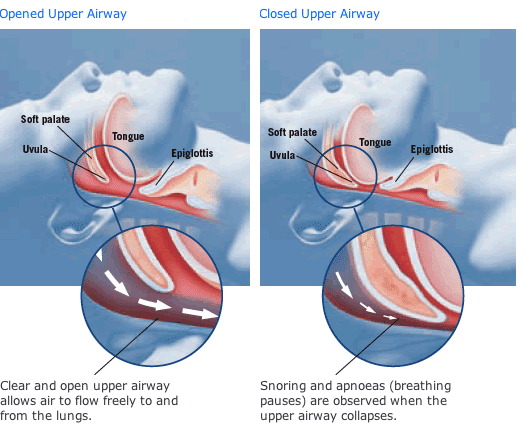
Snoring is the sound produced when the soft tissues in the upper airway vibrate during inspiration and/or expiration. It suggests narrowing of the air passage during sleep with increased resistance to airflow. Treatable causes of snoring includes obesity, smoking, alcohol or benzodiazepines (sleeping pills) use near bedtime, nasal congestion, or craniofacial abnormalities.
Our body compensates by increasing our respiratory drive to maintain sufficient ventilation in the lungs for oxygenation and removal of carbon dioxide from our blood. This increased respiratory effort may cause transient arousals and symptoms of poor sleep. The air flow limitation may progressively worsen and eventually result in cessations of respiration, known as obstructive apnea or shallow/slow breathing known as hypopnoea. This is known as Obstructive Sleep Apnoea (OSA). Not everyone with snoring has or will develop OSA.
It is generally recommended to attend the consultation with your sleeping partner if possible, because they may have greater insight into the problem!
What are symptoms and signs to suggest Obstructive Sleep Apnoea?
The diagnosis of OSA is based upon the presence of symptoms, as well as the frequency of apneas, hypopneas and arousals during sleep.
Any or none of the following symptoms may be present to suggest OSA:
- Episodes of breathing cessation usually manifesting as periods of silence terminated by loud resuscitative snoring
- Awakening with a sensation of choking or gasping
- Restless sleep with tossing and turning, or insomnia with frequent awakenings
- Excessive daytime sleepiness, usually quantified with the Epworth Sleepiness Scale.
- Others include: impaired concentration, mood changes, morning headaches
The following clinical features may also suggest OSA:
- Obesity
- Large neck circumference
- Narrow or “crowded” airway
- Cardiovascular disease or arrhythmias
- Systemic or pulmonary hypertension, or right heart failure
- Cerebrovascular disease encompassing stroke and transient ischaemic attacks
What are the tests for diagnosing Obstructive Sleep Apnoea?
A full history and physical examination, of the ears, nose and throat will be performed to identify structural abnormalities and exclude coexisting diseases.
A sleep study or polysomnography may often be required to diagnose OSA.
Blood tests may be required in rare occasions to exclude endocrine causes such as suspected acromegaly or hypothyroidism.
What are the consequences of untreated snoring and Obstructive Sleep Apnoea?
Snoring alone usually has no direct impact on the snorer’s health (although sleeping partners may suffer from poor sleep, daytime sleepiness and marital dissatisfaction).
If snoring is a sign of OSA, then the condition warrants medical attention.
OSA is associated with impaired daytime function, fatigue, inattention and increase the likelihood of errors and accidents. Road traffic accidents are two to three times more common among patients with OSA than without OSA.
Patients with untreated severe OSA are known to have 3-6 times increased risk of all-cause mortality compared to individuals without OSA. Untreated OSA is also associated with the development of heart disease, heart failure, night-time cardiac death, and perioperative cardiorespiratory complications. OSA is also associated with diabetes.
What are some of the treatment options for Snoring and Obstructive Sleep Apnoea?
Treatment of snoring is recommended to minimise sleep disturbance to sleeping partners and to relieve the patient of any associated embarrassment. Lifestyle interventions include physical exercise, dietary modification, weight loss, smoking cessation, alcohol abstinence, and sleeping in the lateral position. Medical therapy includes nasal decongestants (temporary), nasal steroid sprays, external nasal dilators, and continuous positive airway pressure (CPAP), depending on the underlying aetiology and co-morbidities. Surgery is usually the last resort for refractory cases.
On the other hand, there are no medicines of proven value in the treatment of OSA. Apart from the aforementioned lifestyle interventions, OSA is best treated with CPAP, which is a device which blows a gentle stream of air through the nose at night via a mask or oral appliance. Patients with OSA will often be advised to use the CPAP device throughout sleep on a long term basis.
Surgical procedures for OSA are usually reserved for patients who have failed, declined or are unsuitable for a trial of conservative therapy with CPAP. Surgery would also be indicated in patients with OSA who have a surgically correctable obstructing lesion. This involves the removal of some of the tissues in the airways (soft palate, uvula, tongue reduction, etc) to reduce the airway obstruction, but as with any other surgery, the risks need to be weighed against the benefits.
Please contact us if you have further enquiry on Snoring and Obstructive Sleep Apnea or Request an appointment to see our ENT specialist